Colorectal
Hurstville Private Hospital GP Bulletin
June - July 2019
Not so long ago, surgeons could push operative boundaries, such as laparoscopic techniques, in the absence of iron-clad evidence demonstrating benefit. The introduction of laparoscopy revolutionised recovery following cholecystectomy, and will never be subjected to the standard of scrutiny accorded level 1 evidence. The rate of surgical uptake of laparoscopic cholecystectomy preceded availability of evidence. We anticipated good outcomes compared with open cholecystectomy, and fortuitously, the passage of time has proven these expectations well founded.
In more recent times surgical bravado has been tempered, and attitudes to new technology are no longer quite so cavalier. In part, this may be due to the expense incurred. After all, a robotic program requires a capital investment in the order of several million dollars, and annual expenses of consumables and maintenance, which rapidly accrue. So now more than before, costs confound scrutiny of practice and the careful consideration of patient benefit that would precede widespread adoption of these new technologies.
Laparoscopic techniques in colorectal surgery have been associated with shortened recovery time and hospital stay, less postoperative pain and faster return to bowel function compared with the traditional open approach.(1-3) Around the world, minimally invasive techniques are rapidly becoming the norm with consistently demonstrated postoperative patient benefits.(4, 5)
However, the learning curve for laparoscopic colorectal surgery is steep, with geographic variation in uptake and conversion rate despite advances in equipment design, optics and the widespread adoption of laparoscopy.(6) Laparoscopic colorectal surgery is challenging, particularly when confined to the pelvis.(7) Reliance on the surgical assistant to obtain an adequate two dimensional view, and limited dexterity resulting from instrument rigidity, add to operative complexity.(8) Surgical ergonomics are restricted most when accurate dissection is most critical, for instance, in planes adjacent to autonomic nerve plexii.
Other factors that complicate laparoscopic colorectal surgery include patient and pathology related variables. Factors that place patients at higher risk of conversion and peri-operative complications, such as anastomotic dehiscence, include male gender, high body-mass index, neoadjuvant chemoradiation, the anatomically narrow pelvis, re-do abdomino-pelvic surgery, bulky or fixed disease, and low rectal tumours.(9, 10) Laparoscopy in this cohort is difficult because of instrument crowding, and a compromised and limited visual field. Patients are exposed to specific anaesthetic and operative risks related to extreme positioning and prolonged pneumoperitoneum, increasing postoperative complications. Conversion from laparoscopic to open surgery is independently associated with increased rates of morbidity, blood transfusions, wound infections and length of stay.(2, 11, 12)
The robotic platform offers multiple technical operative advantages to the surgeon faced with these challenges. The surgeon-controlled stable 3-D visual field, improved freedom of movement, and precision operating are robotic tools, which enhance surgical ability, and add to patient safety. Robotic surgical systems are designed to compensate for the limitations of laparoscopic surgery, by providing the level of dexterity surgeons enjoy in open procedures, yet still maintaining the post-operative benefits of minimally invasive techniques.
Of course, robotic systems have their limitations. The absence of haptic feedback is frequently cited as a limitation of robotic surgery. The lack of tactile sensation could predispose to iatrogenic trauma related to excessive traction on tissues. Despite this potential risk, there has been no increase of iatrogenic colonic trauma reported in the literature. Appropriate emphasis on the surgical appreciation of visual cues during robotic training, improved 3-D operative view and precise robotic dissection likely compensate for this tactile disconnect.
Since the first robotic colectomy in 2002,(13) a number of case series and prospective studies have proved the feasibility and safety of this approach.(14, 15) At first glance, the advantages appear operator-focused, namely increased manoeuvrability, a stable 3-D visual field, manual dexterity and superior ergonomics. However, robotic colorectal surgery has also been shown to be associated with higher rates of sphincter-preservation, reduced blood loss, fewer conversions, and shorter hospital stay.(16) There is evidence that robotic colorectal surgery results in improved post-operative sexual, and to some extent, urinary function.(17, 18)
Operative times are longer in the majority of the published literature comparing robotic with laparoscopic approaches, but docking and console time should improve with the learning curve and expertise of the theatre support team.(19, 20)
Up until 2015, the colorectal literature supported laparoscopy for the management of rectal cancer. However, two recent randomised controlled trials powered for non-inferiority have failed to demonstrate that the oncological outcomes of laparoscopic rectal cancer surgery were equivalent to open resection.(21, 22) In their wake, some centres adopted a hybrid operative approach, performing the mesorectal dissection through a low midline laparotomy or Pfannenstiel incision, compromising the benefits of a minimally invasive approach to achieve optimal oncological outcomes.
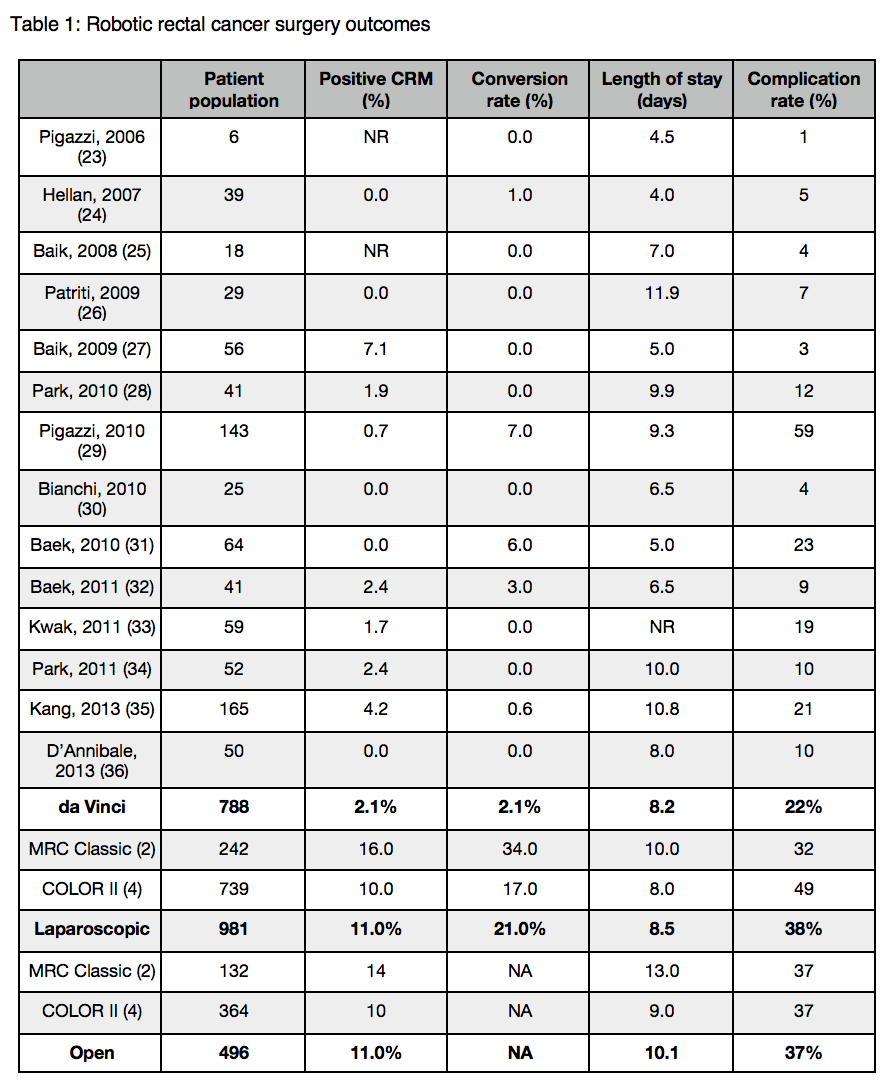
Currently, routine laparoscopic surgery for rectal cancer can no longer be supported. Although robotic rectal surgery is yet to demonstrate superiority in lymph node yield and the rate of positive circumferential resection margin, initial data is promising with a trend toward higher rates of clear margins (see table 1). Employing robotic techniques for rectal cancer will preserve the patient benefits of minimally invasive surgery, with an increasing body of evidence to demonstrate preserved oncological outcomes compared with open or laparoscopic surgery. Of course, long-term outcomes are awaited.
Whether the robot’s technical advantages will translate into long-term oncological benefits remains to be seen. During this period of surgical equipoise, ethical care for our patients is dependent on our adherence to the idiom that should govern any clinical practice in adopting a new technique – the constant improvement of patient care, in response to an honest and robust appraisal of outcomes.
Ethical adoption of robotics can be facilitated by a structured training framework. Although the learning curve for robotic surgery appears to be a shorter journey than for laparoscopy,(37-41) the surgeon needs specialised understanding of the robotic platform to manipulate the instruments and trouble-shoot technical pitfalls. The unstructured ad-hoc self-education that accompanied early adoption of laparoscopic cholecystectomy was associated with an initially high rate of bile duct injuries, and it’s robotic corollary should not be tolerated in today’s society.
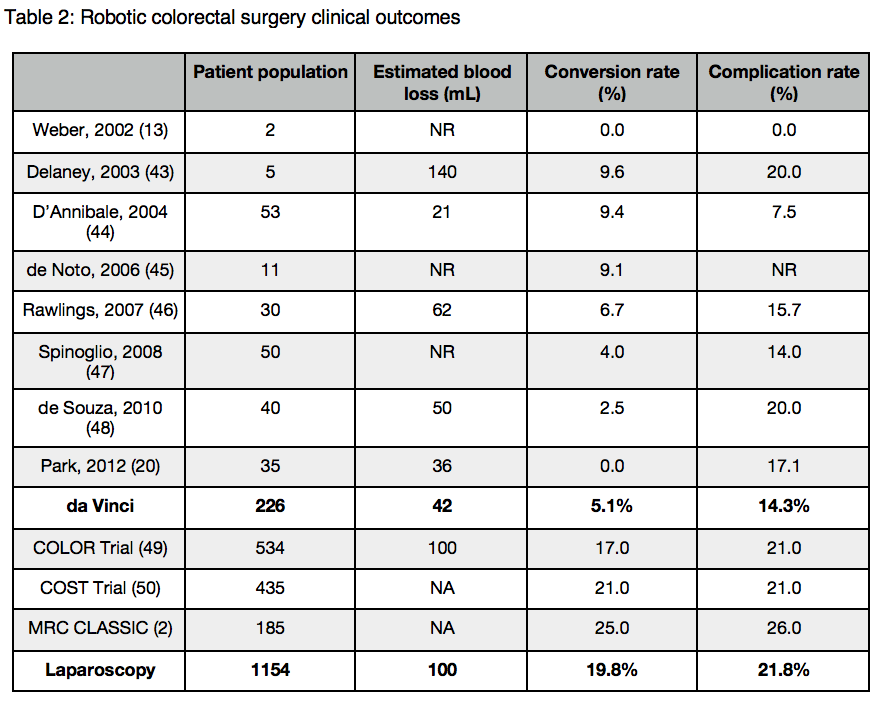
The cost of robotic surgery, more so than with other surgical innovations, overshadows our ability to adopt the technology and scientifically assess its role. However, assessing cost-effectiveness in surgery can be complicated. For example, it is hard to account for the cost savings in minimising peri-operative complications and transfusion requirements. The increased length of stay, readmission rate, imaging studies, interventional radiological procedures, additional operations and office visits associated with anastomotic leakage has been estimated to amount to more than $28.6 million in additional costs and 9500 days in prolonged hospitalisation per 1000 patients undergoing colorectal surgery.(42) Robotic techniques appear to reduce complication rate and have the potential to offset the initial costs involved in the index procedure (see table 2).
Modern medicine is capable of supporting chronic disease, maintaining quality of life and extending longevity in our ageing population. Increasingly sophisticated investigations and treatments delivered in the context of individualised care plans carry an economic burden. Doctors are not only asked to assess the clinical benefits of novel treatments compared with standard management, but to weigh the improvement in outcomes against the financial burden they often impose. We have seen this particularly in the introduction of novel surgical technologies such as the robot.
Robotic colorectal surgery holds great promise. It may prove to overcome the limitations of laparoscopy in achieving the benefits of minimally invasive surgery, without compromising the oncological standards of open resection. So far, the literature has demonstrated the safe application of robotic techniques to benign and malignant indications in colorectal surgery. We all await larger definitive randomised trials to assess its impact on long-term oncological outcomes in cancer surgery. Rather than dismiss it prematurely as an expensive gimmick, we should permit robotic surgery the test of time and scientific scrutiny.
Dr Kim-Chi Phan-Thien, BSc(Med), MBBS(Hons), MS, FRACS
Dr Kim Phan-Thien graduated with honours from the University of New South Wales and obtained her Master of Surgery from the University of Sydney. She completed her surgical training and colorectal fellowship through Liverpool and St George Hospitals. Kim is a fellow of the Royal Australasian College of Surgeons and a member of the Colorectal Surgical Society of Australia and New Zealand.
Kim has a particular interest in minimally invasive (transanal, laparoscopic and robotic) techniques for the treatment of colorectal conditions. As an experienced robotic surgeon, she is a da Vinci accredited robotic proctor and helps with the training of surgeons in robotic techniques.
Kim's clinical practice encompasses colorectal cancer, inflammatory bowel disease and anorectal pathology. To provide wholistic care for her female patients with endometriosis and functional problems of the pelvic floor, she collaborates with Endogynaecology and Urogynaecology specialists. As a member of the St George Pelvic Floor Unit, she helps manage colorectal problems affecting women during their pregnancy and following delivery.
Kim has a passion for teaching and research. She has been recognised by the Academy of Surgical Educators of the Royal Australasian College of Surgeons and the University of New South Wales for her contributions to medical education. Kim has been an invited speaker at scientific meetings. Her past research collaborations in Lynch syndrome have led to the Cancer Institute NSW Premier’s Award for Excellence in Translational Cancer Research.
Kim is a VMO Colorectal Surgeon at St George Hospital, and has appointments at Hurstville and St George Private Hospitals. She consults at Kogarah, Hurstville and Miranda.
CONTACT DETAILS
T (02) 8566 1000
Suite 3, Level 2
Hurstville Private Hospital
37 Gloucester Road
Hurstville NSW 2220
References:
1. Bonjer HJ, Hop WC, Nelson H, Sargent DJ, Lacy AM, Castells A, et al. Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Archives of surgery. 2007;142(3):298-303.
2. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365(9472):1718-26.
3. Leung KL, Kwok SP, Lam SC, Lee JF, Yiu RY, Ng SS, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet. 2004;363(9416):1187-92.
4. van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. The lancet oncology. 2013;14(3):210-8.
5. Zhao JH, Sun JX, Huang XZ, Gao P, Chen XW, Song YX, et al. Meta-analysis of the laparoscopic versus open colorectal surgery within fast track surgery. Int J Colorectal Dis. 2016;31(3):613-22.
6. Reames BN, Sheetz KH, Waits SA, Dimick JB, Regenbogen SE. Geographic variation in use of laparoscopic colectomy for colon cancer. J Clin Oncol. 2014;32(32):3667-72.
7. Bege T, Lelong B, Esterni B, Turrini O, Guiramand J, Francon D, et al. The learning curve for the laparoscopic approach to conservative mesorectal excision for rectal cancer: lessons drawn from a single institution's experience. Annals of surgery. 2010;251(2):249-53.
8. Berguer R, Rab GT, Abu-Ghaida H, Alarcon A, Chung J. A comparison of surgeons' posture during laparoscopic and open surgical procedures. Surg Endosc. 1997;11(2):139-42.
9. Hemandas AK, Abdelrahman T, Flashman KG, Skull AJ, Senapati A, O'Leary DP, et al. Laparoscopic colorectal surgery produces better outcomes for high risk cancer patients compared to open surgery. Annals of surgery. 2010;252(1):84-9.
10. Tan PY, Stephens JH, Rieger NA, Hewett PJ. Laparoscopically assisted colectomy: a study of risk factors and predictors of open conversion. Surg Endosc. 2008;22(7):1708-14.
11. Agha A, Furst A, Iesalnieks I, Fichtner-Feigl S, Ghali N, Krenz D, et al. Conversion rate in 300 laparoscopic rectal resections and its influence on morbidity and oncological outcome. Int J Colorectal Dis. 2008;23(4):409-17.
12. Yamamoto S, Fukunaga M, Miyajima N, Okuda J, Konishi F, Watanabe M, et al. Impact of conversion on surgical outcomes after laparoscopic operation for rectal carcinoma: a retrospective study of 1,073 patients. J Am Coll Surg. 2009;208(3):383-9.
13. Weber PA, Merola S, Wasielewski A, Ballantyne GH. Telerobotic-assisted laparoscopic right and sigmoid colectomies for benign disease. Dis Colon Rectum. 2002;45(12):1689-94; discussion 95-6.
14. Abodeely A, Lagares-Garcia JA, Duron V, Vrees M. Safety and learning curve in robotic colorectal surgery. J Robot Surg. 2010;4(3):161-5.
15. Collinson FJ, Jayne DG, Pigazzi A, Tsang C, Barrie JM, Edlin R, et al. An international, multicentre, prospective, randomised, controlled, unblinded, parallel-group trial of robotic-assisted versus standard laparoscopic surgery for the curative treatment of rectal cancer. Int J Colorectal Dis. 2012;27(2):233-41.
16. Ahmed J, Cao H, Panteleimonitis S, Khan J, Parvaiz A. Robotic vs laparoscopic rectal surgery in high-risk patients. Colorectal Dis. 2017;19(12):1092-9.
17. Broholm M, Pommergaard HC, Gogenur I. Possible benefits of robot-assisted rectal cancer surgery regarding urological and sexual dysfunction: a systematic review and meta-analysis. Colorectal Dis. 2015;17(5):375-81.
18. Kim JY, Kim NK, Lee KY, Hur H, Min BS, Kim JH. A comparative study of voiding and sexual function after total mesorectal excision with autonomic nerve preservation for rectal cancer: laparoscopic versus robotic surgery. Ann Surg Oncol. 2012;19(8):2485-93.
19. Keller DS, Senagore AJ, Lawrence JK, Champagne BJ, Delaney CP. Comparative effectiveness of laparoscopic versus robot-assisted colorectal resection. Surg Endosc. 2014;28(1):212-21.
20. Park JS, Choi GS, Park SY, Kim HJ, Ryuk JP. Randomized clinical trial of robot-assisted versus standard laparoscopic right colectomy. Br J Surg. 2012;99(9):1219-26.
21. Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, et al. Effect of Laparoscopic-Assisted Resection vs Open Resection on Pathological Outcomes in Rectal Cancer: The ALaCaRT Randomized Clinical Trial. JAMA. 2015;314(13):1356-63.
22. Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, et al. Effect of Laparoscopic-Assisted Resection vs Open Resection of Stage II or III Rectal Cancer on Pathologic Outcomes: The ACOSOG Z6051 Randomized Clinical Trial. JAMA. 2015;314(13):1346-55.
23. Pigazzi A, Ellenhorn JD, Ballantyne GH, Paz IB. Robotic-assisted laparoscopic low anterior resection with total mesorectal excision for rectal cancer. Surg Endosc. 2006;20(10):1521-5.
24. Hellan M, Anderson C, Ellenhorn JD, Paz B, Pigazzi A. Short-term outcomes after robotic-assisted total mesorectal excision for rectal cancer. Ann Surg Oncol. 2007;14(11):3168-73.
25. Baik SH, Ko YT, Kang CM, Lee WJ, Kim NK, Sohn SK, et al. Robotic tumor-specific mesorectal excision of rectal cancer: short-term outcome of a pilot randomized trial. Surg Endosc. 2008;22(7):1601-8.
26. Patriti A, Ceccarelli G, Bartoli A, Spaziani A, Biancafarina A, Casciola L. Short- and medium-term outcome of robot-assisted and traditional laparoscopic rectal resection. JSLS. 2009;13(2):176-83.
27. Baik SH, Kwon HY, Kim JS, Hur H, Sohn SK, Cho CH, et al. Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol. 2009;16(6):1480-7.
28. Park JS, Choi GS, Lim KH, Jang YS, Jun SH. Robotic-assisted versus laparoscopic surgery for low rectal cancer: case-matched analysis of short-term outcomes. Ann Surg Oncol. 2010;17(12):3195-202.
29. Pigazzi A, Luca F, Patriti A, Valvo M, Ceccarelli G, Casciola L, et al. Multicentric study on robotic tumor-specific mesorectal excision for the treatment of rectal cancer. Ann Surg Oncol. 2010;17(6):1614-20.
30. Bianchi PP, Ceriani C, Locatelli A, Spinoglio G, Zampino MG, Sonzogni A, et al. Robotic versus laparoscopic total mesorectal excision for rectal cancer: a comparative analysis of oncological safety and short-term outcomes. Surg Endosc. 2010;24(11):2888-94.
31. Baek JH, McKenzie S, Garcia-Aguilar J, Pigazzi A. Oncologic outcomes of robotic-assisted total mesorectal excision for the treatment of rectal cancer. Annals of surgery. 2010;251(5):882-6.
32. Baek JH, Pastor C, Pigazzi A. Robotic and laparoscopic total mesorectal excision for rectal cancer: a case-matched study. Surg Endosc. 2011;25(2):521-5.
33. Kwak JM, Kim SH, Kim J, Son DN, Baek SJ, Cho JS. Robotic vs laparoscopic resection of rectal cancer: short-term outcomes of a case-control study. Dis Colon Rectum. 2011;54(2):151-6.
34. Park JS, Choi GS, Lim KH, Jang YS, Jun SH. S052: a comparison of robot-assisted, laparoscopic, and open surgery in the treatment of rectal cancer. Surg Endosc. 2011;25(1):240-8.
35. Kang J, Yoon KJ, Min BS, Hur H, Baik SH, Kim NK, et al. The impact of robotic surgery for mid and low rectal cancer: a case-matched analysis of a 3-arm comparison--open, laparoscopic, and robotic surgery. Annals of surgery. 2013;257(1):95-101.
36. D'Annibale A, Pernazza G, Monsellato I, Pende V, Lucandri G, Mazzocchi P, et al. Total mesorectal excision: a comparison of oncological and functional outcomes between robotic and laparoscopic surgery for rectal cancer. Surg Endosc. 2013;27(6):1887-95.
37. Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011;25(3):855-60.
38. Shaw DD, Wright M, Taylor L, Bertelson NL, Shashidharan M, Menon P, et al. Robotic Colorectal Surgery Learning Curve and Case Complexity. Journal of laparoendoscopic & advanced surgical techniques Part A. 2018;28(10):1163-8.
39. Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW, Jr. The learning curve for laparoscopic colorectal surgery. Preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Archives of surgery. 1997;132(1):41-4; discussion 5.
40. Dincler S, Koller MT, Steurer J, Bachmann LM, Christen D, Buchmann P. Multidimensional analysis of learning curves in laparoscopic sigmoid resection: eight-year results. Dis Colon Rectum. 2003;46(10):1371-8; discussion 8-9.
41. Schlachta CM, Mamazza J, Seshadri PA, Cadeddu M, Gregoire R, Poulin EC. Defining a learning curve for laparoscopic colorectal resections. Dis Colon Rectum. 2001;44(2):217-22.
42. Hammond J, Lim S, Wan Y, Gao X, Patkar A. The burden of gastrointestinal anastomotic leaks: an evaluation of clinical and economic outcomes. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2014;18(6):1176-85.
43. Delaney CP, Lynch AC, Senagore AJ, Fazio VW. Comparison of robotically performed and traditional laparoscopic colorectal surgery. Dis Colon Rectum. 2003;46(12):1633-9.
44. D'Annibale A, Morpurgo E, Fiscon V, Trevisan P, Sovernigo G, Orsini C, et al. Robotic and laparoscopic surgery for treatment of colorectal diseases. Dis Colon Rectum. 2004;47(12):2162-8.
45. DeNoto G, Rubach E, Ravikumar TS. A standardized technique for robotically performed sigmoid colectomy. Journal of laparoendoscopic & advanced surgical techniques Part A. 2006;16(6):551-6.
46. Rawlings AL, Woodland JH, Vegunta RK, Crawford DL. Robotic versus laparoscopic colectomy. Surg Endosc. 2007;21(10):1701-8.
47. Spinoglio G, Summa M, Priora F, Quarati R, Testa S. Robotic colorectal surgery: first 50 cases experience. Dis Colon Rectum. 2008;51(11):1627-32.
48. deSouza AL, Prasad LM, Marecik SJ, Blumetti J, Park JJ, Zimmern A, et al. Total mesorectal excision for rectal cancer: the potential advantage of robotic assistance. Dis Colon Rectum. 2010;53(12):1611-7.
49. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. The lancet oncology. 2005;6(7):477-84.
50. Clinical Outcomes of Surgical Therapy Study G, Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350(20):2050-9.